Research Article | Open Access
Self-medication with antibiotics and its associated factors among university students: a cross-sectional study
Shams Ullah1, Qurish Ali1, Dost Mohammad1, Anisa1, Talha Ahmed1, Muhammad Arif1, Riaz Ahmed1, Muhammad Farooq1, Abdul Ghafar2, Abdul Wahid3
1Department of Pharmacy, Faculty of Pharmacy and Health Sciences, University of Balochistan, Quetta, Pakistan.
2Department of Pharmacology, Faculty of Pharmacy and Health Sciences, University of Balochistan, Quetta, Pakistan.
3Department of Pharmacy Practice, Faculty of Pharmacy and Health Sciences, University of Balochistan, Quetta, Pakistan.
Correspondence: Abdul Wahid (Department of Pharmacy Practice, Faculty of Pharmacy and Health Sciences, University of Balochistan, Quetta, Pakistan; E-mail: royalbolan@gmail.com).
Asia-Pacific Journal of Pharmacotherapy & Toxicology 2024, 4: 9-17. https://doi.org/10.32948/ajpt.2024.03.20
Received: 27 Feb 2024 | Accepted: 21 Mar 2024 | Published online: 24 Mar 2024
Methods This study was conducted at the University of Balochistan from April to November 2022, to find out the prevalence of self-medication among students through a comprehensive questionnaire covering frequency, reasons, types of medications used, sources of information, and demographic characteristics. SPSS version 21 was used to analyze the data.
Results In this study, a total of 730 participants took part, resulting in a response rate of (708) 97%. The average age of the study participants was 22.78 ± 2.758 years. The study found that most participants were male (69.5%), with the highest representation from third-year students in the biological sciences field (30.5%), primarily residing in hostels (59.3%) and receiving monthly allowances between 10000-15000 (54.2%). Factors such as gender, marital status, field of study in biological and natural sciences, residing in a hostel, absence of family members in the health profession, and specific monthly allowance ranges.
Conclusion The study concluded high rates of self-administration of antibiotics among University of Balochistan students, with factors such as gender, marital status, field of study, hostel residency, family healthcare background, and financial constraints playing significant roles. Urgent interventions are necessary to educate students on the dangers of self-medication.
Key words antibiotics, antibiotic resistance, self-medication, Pakistan
Globally, the prevalence of self-medication ranges from 11.2% to 93.7%, depending on living standards. In developing countries, most people take care of their health problems by using medicines on their own. In Pakistan, the prevalence of self-medication is notably high, up to 85%, with contributing factors including easy access to medicines, lack of healthcare knowledge, and limited access to healthcare facilities [9]. In countries with weak healthcare systems, the existing issue of limited healthcare access has been further exacerbated by the pandemic. Factors such as the quality of the healthcare system, poverty levels, gender, and age contribute to the varying prevalence of self-medication across different regions [10]. Using antibiotics without a doctor's advice often leads to medication errors, including improper dosage, sharing drugs, and prematurely stopping treatment once symptoms improve. These actions can cause problems like drug interactions, other health issues, and develop antibiotic resistance [11]. The rise in antibiotics resistance poses a significant danger to public health, leading to longer hospital stays and increased mortality rates [11, 12]. Studies in Pakistan have shown very high rates of people using antibiotics without a doctor's advice [13, 14]. The accessibility of antibiotics without prescriptions and the lack of regulatory control further burden state and federal healthcare systems [14, 15]. This study aims to investigate and assess the prevalence of self-medication with antibiotics, identify the risk factors contributing to this practice, determine the common symptoms treated through self-medication, and explore the reasons behind antibiotic self-medication. This study is motivated by the growing prevalence of antibiotic resistance and the excessive use of antibiotics during the COVID-19 pandemic in Pakistan.
The current study was a prospective cross-sectional study carried out at the University of Balochistan, Quetta, from April 2021 to November 2021. The University of Balochistan is a public university established in 1974 in Quetta, Balochistan, Pakistan. It has more than 10,000 students, three sub-campuses, 35 different departments, and six faculties. Initially, students from various fields such as Social Sciences, Natural Sciences, and Biological Sciences were approached. Subsequently, a convenience sampling technique was used in the second stage to recruit study participants from different academic departments and years of study.
Data Collection
The data were collected using a comprehensive data collection form designed from previous literature. The data collection form included questions regarding frequency, reasons, types of medications used, sources of information, and demographic characteristics of the study participants. Prior to data collection, a pilot study was conducted on 30 students to ensure that the data collection form was clear, applicable, and understandable to the study population. The data were collected by qualified research assistants using a convenient sampling approach. Participants were briefed on the study objectives, assured of confidentiality, and provided informed consent before completing the questionnaire. Rigorous quality control measures were implemented throughout the data collection process to maintain the integrity and accuracy of the collected data.
Statistical Analysis
SPSS version 21 was used to analyze the data, involving both descriptive and inferential statistics. Frequencies, percentages, means, and standard deviations were calculated to summarize demographic characteristics and self-medication behaviors. Additionally, regression models were employed to identify potential predictors and factors influencing self-medication practices, with a p-value less than 0.05 considered significant.
The overall prevalence of self-medication among university students was found to be 50.1% (Figure 1). However, certain subgroups exhibited higher rates of self-medication. Specifically, male students had a prevalence rate of 63.8%, students in the field of biological sciences had a rate of 63.6%, and students residing in hostels had a rate of 57.9%, while those with a monthly allowance in the range of 5,000-10,000 PKR had the highest prevalence (83.3%) of self-medication as shown in Table 1.
The primary reasons for self-medication included the desire for immediate access without the need to wait (28.8%), perceiving the disease as not serious (27.1%), lack of trust in healthcare professionals (20.3%), poor economic status (18.6%), and past personal experiences (5.1%) (Figure 2). In terms of the specific complaints that led individuals to self-medicate with antibiotics, gastric problems accounted for 28.2%, dental issues for 16.4%, and renal pain for 13.7% of the cases, as shown in Table 2.
The majority of individuals obtained antibiotics from different sources: community pharmacies (47.5%), friends and relatives (27.1%), and previous doctors' prescriptions (15.3%) (Figure 3). Amoxicillin was the most frequently used antibiotic (30.4%), followed by Co-Amoxiclav (12.1%), Ampicillin (10.1%), and Azithromycin (8.7%), as shown in Table 3.
Factors associated with self-medication with antibiotics
To identify the factors associated with self-medication with antibiotics, both univariate and multivariate binary logistic regression analyses were conducted. In the univariate analysis, several variables showed significant associations with self-medication. These included gender (male) with an odds ratio (OR=1.497, p-value=0.000), marital status (married) (OR=0.2663, p-value=0.000), field of study (biological sciences) (OR=1.514, p-value=0.001), year of study (3rd year, 4th year, and 5th year) with respective odds and p-values (OR=0.0701, p-value=0.010, OR=1.667, p-value=0.015, and OR=0.571, p-value=0.002), and monthly allowance >20,000 PKR (OR=0.290, p-value=0.000), all of which had significant associations with self-medication with antibiotics.
Following the univariate analysis, the significant variables were further analyzed using multivariate binary logistic regression analysis, considering the adjusted odds ratios. In this analysis, the variables that retained their significance as risk factors for self-medication with antibiotics were male gender (OR=99.998, p-value=0.000), marital status (married) (OR=10.665, p-value=0.000), field of study (biological sciences) (OR=24.873, p-value=0.000), field of study (natural sciences) (OR=12.587, p-value=0.000), year of study (2nd year and 3rd year) with respective ORs of 0.295 and 0.035, and corresponding p-values of 0.033 and 0.000, residence (hostel) (OR=43.316, p-value=0.000), absence of family members in health (OR=0.012, p-value=0.000), and monthly allowance (10,000-15,000 PKR, 15,000-20,000 PKR, and >20,000 PKR) with respective ORs of 0.004, 0.001, and 0.0000, and corresponding p-values of 0.000, 0.000, and 0.000. Table 4 provides insights into the factors associated with self-medication with antibiotics, both univariate and multivariate.
|
Table 1. Socio-demographics of the study participants and self-medication with antibiotics. |
||||
|
Items |
Variables |
Total No. (%) |
Without Antibiotics, No. (%) |
With Antibiotics, No. (%) |
|
Age |
15-20 |
72 (10.2) |
36 (50.0) |
36 (50.0) |
|
21-25 |
540 (76.3) |
269 (49.8) |
271 (50.2) |
|
|
26-30 |
72 (10.2) |
15 (20.8) |
57 (79.2) |
|
|
<30 |
24 (3.4) |
14(58.3) |
10(41.7) |
|
|
Gender |
Male |
492 (69.5) |
178 (36.2) |
314 (63.8) |
|
Female |
215 (30.5) |
156 (46.7) |
60 (27.8) |
|
|
Marital status |
Single |
660 (93.2) |
296 (44.8) |
364 (55.2) |
|
Married |
48 (6.8) |
38 (79.2) |
10 (2.8) |
|
|
Field of Study |
Social Sciences |
192 (27.1) |
132 (68.8) |
60 (31.3) |
|
Natural Sciences |
252 (35.6) |
106 (42.1) |
146 (57.9) |
|
|
Biological Sciences |
264(37.3) |
96(36.4) |
168(63.6) |
|
|
Year of Study
|
1st year |
108 (15.3) |
24 (22.2) |
84 (77.8) |
|
2nd year |
156 (22.0) |
82 (52.6) |
74 (47.4) |
|
|
3rd year |
216 (30.5) |
127 (58.8) |
89 (41.2) |
|
|
4th year |
96 (13.6) |
36 (37.5) |
60 (62.5) |
|
|
5th year |
132 (18.6) |
65 (49.2) |
67 (50.8) |
|
|
Residence |
Home |
288 (40.7) |
157 (54.5) |
131 (45.5) |
|
Hostel |
420 (59.3) |
177 (42.1) |
243 (57.9) |
|
|
Family member in Health |
Yes |
96 (13.6) |
72 (75.0) |
24 (25.0) |
|
No |
612 (86.4) |
262 (42.8) |
350 (57.2) |
|
|
Monthly Allowance
|
5000-10000 |
72 (10.02) |
12 (16.7) |
60 (83.3) |
|
10000-15000 |
384 (54.2) |
187 (48.7) |
197 (51.3) |
|
|
15000-20000 |
132 (18.6) |
60 (45.5) |
72 (54.5) |
|
|
>20000 |
120(16.9) |
75(62.5) |
45(37.5) |
|
|
Table 2. Reasons and complaints for self-medication with antibiotics. |
|||
|
Items |
Classification |
Frequency |
Percentage (%) |
|
Reasons |
Poor economic status |
132 |
18.6 |
|
Lack of trust on Doctors |
144 |
20.3 |
|
|
Emergency use and no waiting |
204 |
28.8 |
|
|
The disease was not serious |
192 |
27.1 |
|
|
My own previous experience |
36 |
5.1 |
|
|
Complaints |
Allergy |
82 |
11.6 |
|
Fever |
24 |
3.4 |
|
|
Flu/cough |
12 |
1.7 |
|
|
Gastric problem |
200 |
28.2 |
|
|
Skin infection |
72 |
10.2 |
|
|
Infection and wounds |
57 |
8.1 |
|
|
Dental issues |
116 |
16.4 |
|
|
Renal pain |
97 |
13.7 |
|
|
Sore throat |
48 |
6.8 |
|
|
Table 3. Types and source of antibiotics used for self-medication. |
|||
|
Items |
Classification |
Frequency |
Percentage (%) |
|
Sources of getting Antibiotics |
Community Pharmacy |
336 |
47.5 |
|
Friends and relatives |
192 |
27.1 |
|
|
Internet and mobile App |
36 |
5.1 |
|
|
Previous Doctor prescription |
108 |
15.3 |
|
|
Previous left over |
36 |
5.1 |
|
|
Antibiotics used for Self medication |
Amoxicillin |
168 |
30.4 |
|
Ampicillin |
56 |
10.1 |
|
|
Amoxicillin + calvanic acid |
67 |
12.1 |
|
|
Azithromycin |
48 |
8.7 |
|
|
Cephradine |
24 |
4.3 |
|
|
Ciprofloxacin |
24 |
4.3 |
|
|
Levofloxacin |
16 |
2.9 |
|
|
Moxifloxacin |
18 |
3.2 |
|
|
Cefixime |
18 |
3.2 |
|
|
Clarithromycin |
30 |
5.4 |
|
|
Erythromycin |
36 |
6.5 |
|
|
Doxicyclin |
26 |
4.7 |
|
|
Cephalexin |
20 |
3.6 |
|
|
Table 4. Risk factors associated with self-medication using antibiotics. |
|||||||
|
Variables |
Self-medication with Antibiotics |
Univariate analysis |
Multivariate analysis |
||||
|
No No. (%) |
Yes No. (%) |
OR (95%CI) |
p-value |
OR (95%CI) |
p-value |
||
|
Age
|
15-20 |
36 (50.0) |
36 (50.0) |
Referent |
|
|
|
|
21-25 |
269 (49.8) |
271 (50.2) |
1.007 (0.616-1.647) |
0.976 |
|
|
|
|
26-30 |
36 (47.2) |
38 (52.8) |
1.118 (0.581-2.149) |
0.739 |
|
|
|
|
<30 |
14 (58.3) |
10 (41.7) |
0.714 (0.281-1.817) |
0.480 |
|
|
|
|
Gender
|
Male |
197 (40.0) |
295 (60.0) |
Referent |
|
Referent |
|
|
Female |
156 (46.7) |
60 (27.8) |
1.497 (1.250-1.793) |
0.000 |
99.998 (41.012-243.823) |
0.000 |
|
|
Marital status
|
Single |
313 (47.7) |
345 (52.3) |
Referent |
|
Referent |
|
|
Married |
38 (79.2) |
10 (2.8) |
0.263 (0.131-0.528) |
0.000 |
10.665 (3.062-37.140) |
0.000 |
|
|
Field of Study
|
Social Sciences |
132 (68.8) |
60 (31.3) |
Referent |
|
Referent |
|
|
Natural Sciences |
116 (46.0) |
136 (54.0) |
1.172 (0.915-1.502) |
0.208 |
12.587 (6.134-25.832) |
0.000 |
|
|
Biological Sciences |
105 (39.8) |
159 (63.6) |
1.514 (1.184-1.938) |
0.001 |
24.873 (11.846-52.224) |
0.000 |
|
|
Year of Study
|
1st year |
24 (22.2) |
84 (77.8) |
Referent |
|
Referent |
|
|
2nd year |
82 (52.6) |
74 (47.4) |
0.902 (0.659-1.236) |
0.522 |
0.295 (0.096-0.908) |
0.033 |
|
|
3rd year |
127 (58.8) |
89 (41.2) |
0.0701 (0.534-0.919) |
0.010 |
0.035 (0.009-0.141) |
0.000 |
|
|
4th year |
36 (37.5) |
60 (62.5) |
1.667 (1.103-2.519) |
0.015 |
4.094 (0.954-17.565) |
0.058 |
|
|
5th year |
84 (63.6) |
48 (36.4) |
0.571 (0.401-0.815) |
0.002 |
0.012 (0.003-0.044) |
0.853 |
|
|
Residence |
Home |
158 (54.9) |
130 (45.1) |
Referent |
|
Referent |
0.000 |
|
Hostel |
195 (46.4) |
225 (53.6) |
1.154 (0.953-1.398) |
0.144 |
43.316 (17.947-104.549) |
|
|
|
Family member in Health |
Yes |
72 (75.0) |
24 (25.0) |
Referent |
|
Referent |
|
|
No |
281 (45.9) |
331(54.1) |
0.333 (0.210-0.529) |
0.000 |
0.012 (0.003-0.044) |
0.000 |
|
|
Monthly Allowance
|
5000-10000 |
12 (16.7) |
60 (83.3) |
Referent |
|
Referent |
|
|
10000-15000 |
188 (49.0) |
196 (51.0) |
1.043 (0.854-1.273) |
0.683 |
0.004 (0.001-0.017) |
0.000 |
|
|
15000-20000 |
60 (45.5) |
72 (54.5) |
1.200 (0.852-1.690) |
0.297 |
0.001 (0.000-0.007) |
0.000 |
|
|
>20000 |
93 (77.5) |
27 (22.5) |
0.290 (0.189-0.446) |
0.000 |
0.000 (0.000-0.000) |
0.000 |
|
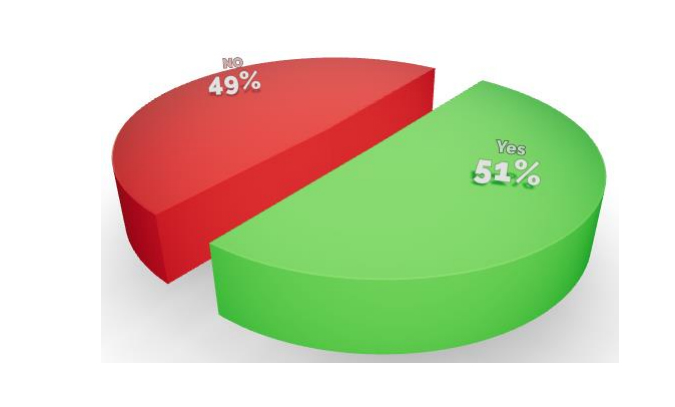 Figure 1. Prevalence of self-medication using antibiotic among university students.
Figure 1. Prevalence of self-medication using antibiotic among university students.
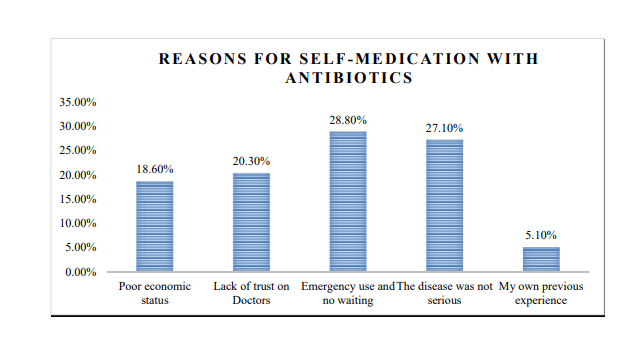 Figure 2. Reasons for self-medication with antibiotics.
Figure 2. Reasons for self-medication with antibiotics.
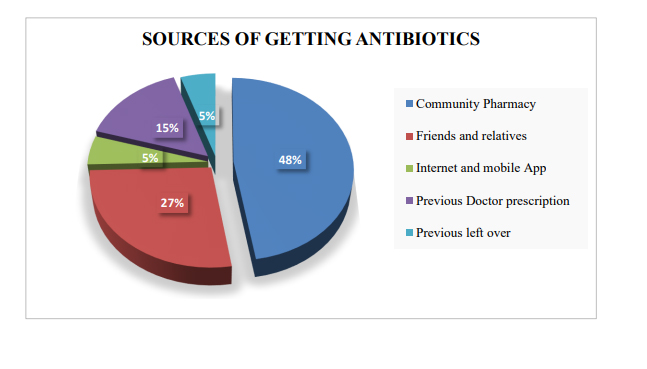 Figure 3. Sources of getting antibiotics.
Figure 3. Sources of getting antibiotics.
The high prevalence of self-medication among university students could be due to difficulties in accessing the healthcare system and insufficient income levels to afford private physicians. In regions where access to formal healthcare services is limited or where private healthcare is financially burdensome, some individuals may opt for self-medication as a more accessible and cost-effective alternative. This phenomenon is particularly prevalent among university students, who may face additional barriers to healthcare access due to their transient living arrangements and limited financial resources [22].
The findings of our study indicate that 28.8% of university students self-administered antibiotics for immediate access without the need to wait, 27.1% thought the illness wasn't serious, 20.3% didn't trust healthcare professionals, 18.6% had financial constraints, and 5.1% relied on their past experiences. Different studies conducted elsewhere have reported similar findings, with people using antibiotics without waiting, having limited financial resources, and relying on their past experiences [23-25]. Overall, these findings demonstrate why university students self-medicate with antibiotics. It's about convenience, their perception of symptom severity, trust in doctors, financial status, and past healthcare experiences. To address these reasons, we need to implement various measures to promote responsible medicine use, ensure easy access to healthcare, and enhance health literacy among students [23-25]. The most common complaints for self-medication with antibiotics were stomach problems (28.2%), dental issues (16.4%), and kidney pain (13.7%). This indicates that people often prefer quick solutions for their health problems, particularly when they believe they can manage them without consulting a doctor [26, 27].
Community pharmacies were the most common source (47.5%), followed by friends and relatives (27.1%), and previous doctors’ prescriptions (15.3%) for obtaining antibiotics. This suggests that antibiotics are easily accessible without a prescription, possibly due to lax regulations or practices in certain regions. Furthermore, there may be a lack of awareness regarding antibiotic resistance and the importance of completing prescribed courses. Factors such as convenience, cost, and trust in informal networks likely drive individuals to obtain antibiotics from these sources. To address this, stricter regulation, public education, and improved access to professional healthcare services are needed. Otherwise, inappropriate antibiotic use could lead to the emergence of antibiotic resistance [28, 29].
The antibiotics Amoxicillin (30.4%), Co-Amoxiclav (12.1%), Ampicillin (10.1%), and Azithromycin (8.7%) were frequently chosen. Similar findings have been reported by other studies conducted elsewhere [30, 31]. Their effectiveness against common bacterial infections and widespread prescription patterns contribute to their use. Several factors influence antibiotic selection, including local prescribing practices, patient allergies, and perceived efficacy. To combat antibiotic resistance and ensure the best patient outcomes, careful and informed antibiotic prescribing practices are necessary [32, 33].
The significant risk factors associated with self-medication with antibiotics included female gender, married marital status, field of study in biological and natural sciences, residing in a hostel, absence of family members in the health profession, and specific monthly allowance ranges. Female gender emerges as a notable risk factor because females are more health-conscious and may be more proactive in seeking out remedies for minor ailments independently, leading to higher rates of self-medication [31, 32]. Cultural factors and experiences related to menstruation or reproductive health may contribute to increased self-medication behaviors among female students, as they seek relief from associated symptoms [34, 35]. The field of study in natural and biological sciences may provide students with better healthcare knowledge, leading to self-diagnosis and self-medication based on their medical knowledge. Additionally, staying in a hostel with friends, previous prescriptions, and having limited financial resources may contribute to increased self-medication behaviors among students [36]. Inadequate facilities or financial limitations may promote students' self-medication as a convenient and cost-effective solution to manage health issues. Lower monthly allowances potentially limit access to professional medical care and prescribed medications [37]. These findings underscore the need for targeted interventions addressing socio-cultural norms, healthcare access, and financial constraints to promote responsible antibiotic use among university students and mitigate the associated risks of self-medication [38].
We thank the dean, Faculty of Pharmacy and Health Sciences University of Balochistan and all the students for their support during this research.
Ethics approval
The ethical committee of Faculty of Pharmacy and Health Sciences University of Balochistan approved the study and written consent was taken from study participants.
Data availability
The Data will be available upon request.
Funding
The authors did not receive any funding or support to report.
Authors’ contribution
Abdul Wahid conceptualized and supervised the study, while Shams Ullah, Qurish Ali, Dost Mohammad, Anisa, Talha Ahmed collected and Muhammad Arif, Riaz Ahmed, Muhammad Farooq, entered the data. Abdul Wahid analyzed the data, and Abdul Ghafar critically reviewed it.
Competing interests
The authors have reported no conflicts of interest.
- Adedeji W: The treasure called antibiotics. Ann Ib Postgrad Med 2016, 14(2): 56-57.
- Loyola Filho AId, Lima-Costa MF, Uchôa E: Bambuí Project: a qualitative approach to self-medication. Cad Saude Publica 2004, 20(6): 1661-1669.
- Elong Ekambi G-A, Okalla Ebongue C, Penda IC, Nnanga Nga E, Mpondo Mpondo E, Eboumbou Moukoko CE: Knowledge, practices and attitudes on antibiotics use in Cameroon: Self-medication and prescription survey among children, adolescents and adults in private pharmacies. PloS one 2019, 14(2): e0212875.
- Högberg LD, Muller A, Zorzet A, Monnet DL, Cars O: Antibiotic use worldwide. Lancet Infect Dis 2014, 14(12): 1179-1180.
- Awad AI, Eltayeb IB, Capps PA: Self-medication practices in Khartoum state, Sudan. Eur J Clin Pharmacol 2006, 62(4): 317-324.
- Elmahi OKO, Musa RAE, Shareef AAH, Omer MEA, Elmahi MAM, Altamih RAA, Mohamed RIH, Alsadig TFM: Perception and practice of self-medication with antibiotics among medical students in Sudanese universities: A cross-sectional study. PloS one 2022, 17(1): e0263067.
- Faraji F, Jalali R, Salari N: The Relationship between Fear of COVID-19 and Self-Medication and the Rate of Antibiotic Use in Patients Referred to COVID-19. Interdiscip Perspect Infect Dis 2022, 2022: 3044371.
- Shrestha AB, Aryal M, Magar JR, Shrestha S, Hossainy L, Rimti FH: The scenario of self-medication practices during the covid-19 pandemic: a systematic review. Ann Med Surg (Lond) 2022, 82: 104482.
- Núñez A, Sreeganga S, Ramaprasad A: Access to Healthcare during COVID-19. Int J Environ Res Public Health 2021, 18(6): 2980.
- Lei X, Jiang H, Liu C, Ferrier A, Mugavin J: Self-medication practice and associated factors among residents in Wuhan, China. Int J Environ Res Public Health 2018, 15(1): 68.
- Sachdev C, Anjankar A, Agrawal J: Self-medication with antibiotics: an element increasing resistance. Cureus 2022, 14(10): e30844.
- Chinemerem Nwobodo D, Ugwu MC, Oliseloke Anie C, Al-Ouqaili MTS, Chinedu Ikem J, Victor Chigozie U, Saki M: Antibiotic resistance: The challenges and some emerging strategies for tackling a global menace. J Clin Lab Anal 2022, 36(9): e24655.
- Bilal M, Haseeb A, Khan MH, Arshad MH, Ladak AA, Niazi SK, Musharraf MD, Manji AA: Self-medication with antibiotics among people dwelling in rural areas of Sindh. J Clin Diagn Res 2016, 10(5): OC08-13.
- Ali I, Khan AU: Self-medication of antibiotics: a perspective on alarming situation in Peshawar, Khyber Pakhtunkhwa, Pakistan. Arch Pharm Pract 2015, 6(3): 68.
- Atif M, Asghar S, Mushtaq I, Malik I, Amin A, Babar ZU, Scahill S: What drives inappropriate use of antibiotics? A mixed methods study from Bahawalpur, Pakistan. Infect Drug Resist 2019, 12: 687-699.
- Chuwa BB, Njau LA, Msigwa KI, Shao E: Prevalence and factors associated with self medication with antibiotics among University students in Moshi Kilimanjaro Tanzania. Afr Health Sci 2021, 21(2): 633-639.
- Ocan M, Bwanga F, Bbosa GS, Bagenda D, Waako P, Ogwal-Okeng J, Obua C: Patterns and predictors of self-medication in northern Uganda. PloS one 2014, 9(3): e92323.
- Donkor ES, Tetteh-Quarcoo PB, Nartey P, Agyeman IO: Self-medication practices with antibiotics among tertiary level students in Accra, Ghana: a cross-sectional study. Int J Environ Res Public Health 2012, 9(10): 3519-3529.
- Shaghaghi A, Asadi M, Allahverdipour H: Predictors of self-medication behavior: a systematic review. Iran J Public Health 2014, 43(2): 136-146.
- Braoios A, Pereira ACS, Bizerra AA, Policarpo OF, Soares NC, Barbosa AdS: [The use of antimicrobial drugs by the population in the city of Jataí, State of Goias, Brazil]. Cien Saude Colet 2013, 18(10): 3055-3060.
- Arnold SR, Straus SE: Interventions to improve antibiotic prescribing practices in ambulatory care. Evidence-Based Child Health 2006, 1(2): 623-690.
- Kifle ZD, Mekuria AB, Anteneh DA, Enyew EF: Self-medication practice and associated factors among private health sciences students in Gondar Town, North West Ethiopia. A Cross-Sectional Study. Inquiry 2021, 58: 00469580211005188.
- Dyar OJ, Hills H, Seitz L-T, Perry A, Ashiru-Oredope D: Assessing the knowledge, attitudes and behaviors of human and animal health students towards antibiotic use and resistance: a pilot cross-sectional study in the UK. Antibiotics 2018, 7(1): 10.
- Sakeena MHF, Bennett AA, Jamshed S, Mohamed F, Herath DR, Gawarammana I, McLachlan AJ: Investigating knowledge regarding antibiotics and antimicrobial resistance among pharmacy students in Sri Lankan universities. BMC Infect Dis 2018, 18(1): 1-11.
- Assar A, Abdelraoof MI, Abdel-Maboud M, Shaker KH, Menshawy A, Swelam AH, Eid M, Khalid R: Knowledge, attitudes, and practices of Egypt’s future physicians towards antimicrobial resistance (KAP-AMR study): a multicenter cross-sectional study. Environ Sci Pollut Res Int 2020, 27(17): 21292-21298.
- Dhedhi NA, Ashraf H, Ansari NB, Iftikhar S: Self-medication among people visiting outpatient clinics of a Tertiary care hospital, Karachi. J Family Med Prim Care 2021, 10(2): 773-779.
- Rathod P, Sharma S, Ukey U, Sonpimpale B, Ughade S, Narlawar U, Gaikwad S, Nair P, Masram P, Pandey S: Prevalence, Pattern, and Reasons for Self-Medication: A Community-Based Cross-Sectional Study From Central India. Cureus 2023, 15(1): e33917.
- Majid Aziz M, Haider F, Rasool MF, Hashmi FK, Bahsir S, Li P, Zhao M, Alshammary TM: Dispensing of non-prescribed antibiotics from community pharmacies of Pakistan: A cross-sectional survey of pharmacy staff’s opinion. Antibiotics 2021, 10(5): 482.
- Ahmad T, Khan FU, Ali S, Rahman AU, Ali Khan S: Assessment of without prescription antibiotic dispensing at community pharmacies in Hazara Division, Pakistan: A simulated client’s study. PLoS One 2022, 17(2): e0263756.
- Gelayee DA: Self-Medication Pattern among Social Science University Students in Northwest Ethiopia. J Pharm (Cairo) 2017, 2017: 8680714.
- Ateshim Y, Bereket B, Major F, Emun Y, Woldai B, Pasha I, Habte E, Russom M: Prevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea: a descriptive cross sectional survey. BMC Public Health 2019, 19(1): 726.
- Aslam A, Gajdács M, Zin CS, Ab Rahman NS, Ahmed SI, Zafar MZ, Jamshed S: Evidence of the practice of self-medication with antibiotics among the lay public in low-and middle-income countries: a scoping review. Antibiotics 2020, 9(9): 597.
- Arboleda Forero V, Cruzate Hernández JP, Yepes Restrepo M, Higuita-Gutiérrez LF: Antibiotic Self-Medication Patterns and Associated Factors in the Context of COVID-19, Medellín, Colombia: A Survey Based Cross Sectional Study. Patient Prefer Adherence 2023, 17: 3057-3066.
- Idris IB, Hamis AA, Bukhori ABM, Hoong DCC, Yusop H, Shaharuddin MA, Fauzi NAFA, Kandayah T: Women’s autonomy in healthcare decision making: a systematic review. BMC Womens Health 2023, 23(1): 643.
- Behzadifar M, Behzadifar M, Aryankhesal A, Ravaghi H, Baradaran HR, Sajadi HS, Khaksarian M, Bragazzi NL: Prevalence of self-medication in university students: systematic review and meta-analysis. East Mediterr Health J 2020, 26(7): 846-857.
- Pandey KR, Yang F, Cagney KA, Smieliauskas F, Meltzer DO, Ruhnke GW: The impact of marital status on health care utilization among Medicare beneficiaries. Medicine 2019, 98(12): e14871.
- Siraj EA, Yayehrad AT, Kassaw AT, Kassahun D, Solomon E, Abdela H, Gizachew G, Awoke E: Self-Medication Prevalence and Factors Associated with Knowledge and Attitude Towards Self-Medication Among Undergraduate Health Science Students at GAMBY Medical and Business College, Bahir Dar, Ethiopia. Patient Prefer Adherence 2022, 16: 3157-3172.
- Araia ZZ, Gebregziabher NK, Mesfun AB: Self medication practice and associated factors among students of Asmara College of Health Sciences, Eritrea: a cross sectional study. J Pharm Policy Pract 2019, 12: 3.
Asia-Pacific Journal of Pharmacotherapy & Toxicology
p-ISSN: 2788-6840
e-ISSN: 2788-6859
 Copyright © Asia Pac J Pharmacother Toxicol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Asia Pac J Pharmacother Toxicol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript