Research Article | Open Access
Evaluating prescription errors and prescribing indicators in the outpatient department of a tertiary care hospital quetta, Pakistan
Shahbaz Babul1, Ghulam Dastagir1, M Pervaiz1, Shoaib Ahmed1, Munir Ahmed1, Shazia Bano1, Mahtab1, Abdul Ghafar2, Abdul Wahid3
1Department of Pharmacy, Faculty of Pharmacy and Health Sciences, University of Balochistan, Quetta, Pakistan.
2Department of Pharmacology, Faculty of Pharmacy and Health Sciences, University of Balochistan, Quetta, Pakistan.
3Department of Pharmacy Practice, Faculty of Pharmacy and Health Sciences, University of Balochistan, Quetta, Pakistan.
Correspondence: Abdul Wahid (Department of Pharmacy Practice, Faculty of Pharmacy and Health Sciences, University of Balochistan, Quetta, Pakistan; E-mail: wahiduob@gmail.com).
Asia-Pacific Journal of Pharmacotherapy & Toxicology 2024, 4: 34-40. https://doi.org/10.32948/ajpt.2024.07.20
Received: 01 Jun 2024 | Accepted: 19 Jul 2024 | Published online: 27 Jul 2024
Methods A cross sectional prospective study was conducted in outpatient department of Sandeman Provencial Hospital, Quetta Pakistan. Nine hundred and sixty prescription were evaluated during the time period September and October 2022 and the world health organization prescribing indicators were used as standard. The data was analyzed using the Statistical Package for the Social Sciences (SPSS) version 20 software. Descriptive statistics were employed to summarize the prescription patterns, including frequencies, percentages, means, and standard deviations.
Results The average drugs per prescription were 3.6 and prescription with antibiotics were 58.3%. Prescription by generic were 10.7%, prescription with injection were 21.9% and prescription with drugs from essential drug list were 61.04%. The most prevalent commission error was the duration of therapy not mentioned 63.4%, followed by frequency not mentioned 27.2%. Other significant errors included dose strength not being specified (25.5%), dose not mentioned 17.0% and dosage form not mentioned 12.6%.
Conclusion The study reveals irrational prescribing practices within the study setting, with the observed values for prescribing indicators deviating from established norms. However, the percentage of encounters involving the prescription of injections fell within the optimal range.
Key words drug interactions, outpatient, prescription errors, prescribing indicators
During the 1990s, the WHO, in partnership with the International Network for Rational Use of Drugs (INRUD), established a set of metrics to assess the performance of healthcare facilities concerning drug utilization [1]. Similarly, the World Health Organization (WHO) established indicators, and including omission and commission errors, to assess prescriptions [5]. Unfortunately, in Pakistan, regulatory bodies have limited or no supervision over prescriptions issued by private and public sector healthcare providers. Consequently, this lack of regulation leads to the inappropriate use of medications, ultimately impacting the well-being of patients [6, 7].
Many studies have been conducted in Pakistan to evaluate, prescription patterns in outpatient settings, due to concerns about inappropriate prescribing practices, medication errors, and patient safety. A similar study was conducted in Karachi which found that high rates of polypharmacy, missing of name gender age patient and prescriber related information on prescriptions, and irrational use of antibiotics [8]. While another similar study was conducted in Quetta which found that a significant proportion of prescriptions lacked essential information, such as patient demographics and diagnosis [9].
This article aimed to explore the importance of prescription patterns, in healthcare settings, particularly in the outpatient department (OPD) of Sandeman Provencial Hospital (SPH) in Quetta, Pakistan. SPH, as a tertiary care hospital, has a critical role in providing specialized care to patients with complex conditions, ensuring responsible drug use, and addressing key public health concerns. By analyzing and understanding prescription practices, healthcare stakeholders can identify areas for improvement, implement evidence-based interventions, and enhance the overall quality and safety of healthcare delivery. This includes optimizing medication management, reducing adverse drug events, and promoting rational drug use.
The present study employed a retrospective cross-sectional design to assess the prescription patterns within the OPD of SPH in Quetta, Pakistan. SPH, is a prominent public tertiary care teaching hospital situated in the capital of Balochistan province (Quetta city), delivers healthcare services to approximately 2.2 million residents of Quetta. Furthermore, as the primary public tertiary care teaching hospital in Balochistan, it serves a broad catchment area encompassing the entire province and the adjacent border regions of Afghanistan and Iran. With an impressive capacity of 800 beds, SPH attends to a staggering 8,000 to 10,000 patients daily. The OPD patients receive check-ups and prescriptions from qualified medical professionals, such as physicians, surgeons, pediatric specialists’, ophthalmologists, dermatologists, psychiatrists, gastroenterologists, chest physicians, general practitioners, and various other specialists.
Study duration and sample size
The study duration spanned two months, specifically September and October 2022. During this period, a total of 1042 prescriptions were randomly selected from the OPD of SPH irrespective of age and gender. However inpatient prescription patients discharge charts and blank prescriptions were excluded from the study as in figure one. The sample size of 960 prescriptions was supposed sufficient to provide a representative sample of prescription patterns during the study period.
Prescription selection and data collection
In the current study trained pharmacy personnel consisting of one assistant pharmacist and one pharmacist from the same hospital retrospectively collected the data on prescribing indicators and errors. The parameters recorded included patient information (e.g., demographics), prescriber details, patient complaints, investigation records, diagnosis notes, and medication details. The study focused on prescriptions from outpatient departments, excluding those of discharged and admitted patients. The tools used in the study underwent rigorous pre-testing to ensure accuracy, reliability, and validity. A multi-step process was employed, involving expert review for content accuracy and clarity, cognitive testing to identify confusing questions, item analysis for accuracy and reliability were performed.
Statistical analysis
The data was analyzed using the Statistical Package for the Social Sciences (SPSS) version 20 software. Descriptive statistics were employed to summarize the prescription patterns, including frequencies, percentages, means, and standard deviations and z test with level of significant p value 0.05.
Prescribing indicators
The World health organization (WHO) prescribing indicators with their optimal values as shown in Table 1 were used in the current study.
Prescription errors
In our study, prescription errors were categorized into two main types: omission errors and commission errors. Omission errors included omission related to patient information (such as name, age, gender, weight, and diagnosis) and prescriber details (including name, address, phone number, qualification, and date). Commission errors, on the other hand, related to inaccuracies in dosage, dosage form, strength, frequency, and treatment duration. Additionally, we examined drug interactions (DIs), classifying them as serious, moderate, and minor. The drug interaction were checked by using www.drugs.com and the book Drug Interaction Facts (2015 edition). It’s important to note that the reported drug-drug interactions focused solely on potential harm, without assessing whether actual harm occurred in exposed patients.
|
Table 1. Prescription indicator and WHO standard values. |
|
|
Prescription Indicator |
WHO standard Values |
|
Average Drugs per Prescription |
1.6-1.8 |
|
Prescriptions with Antibiotics |
20.0-26.8 % |
|
Prescription with Generic |
100 % |
|
Prescription with Injection |
13.4-24.1% |
|
Drug from Essential drug list |
100 % |
Prescription errors
Omission errors: The Table 1 presents the distribution of prescription parameters and their corresponding frequencies and percentages, among the prescription parameters, the lack of patient demographics, including name, age, gender, weight, and diagnosis was observed in 2.6%, 59.9%, 80.0%, 91.7% and 47.9% of prescriptions, respectively were highly significant with a p-value=<0.001. In terms of prescriber details, incomplete information, particularly the absence of prescriber name, qualification, address/ phone number and date was noted in 29.5%, 45.6%, 48.0 and 31.3% of prescriptions, respectively were highly significant with a p-value=<0.001 as shown in Table 3.
Commission errors: The most prevalent commission error was the duration of therapy not mentioned 63.4%, (p-value=<0.05) followed by frequency not mentioned 27.2% (p-value=<0.001). Other significant errors included dose strength not being specified (25.5%) (p-value =<0.05), dose not mentioned 17.0% (p-value=<0.05) and dosage form not mentioned 12.6% (p-value=<0.05) as shown in Table 4.
Errors related to drug-drug interactions: In current study total 871 drug-drug interaction were identified in 960 prescriptions. Among them serious interactions were 16.7%, followed by moderate interactions 42.5%, and minor interactions 31.6% as shown in Table 5 and Figure 2.
|
Table 2. The Prescribing indicators with WHO standard values. |
||||
|
Prescription Indicator |
Total |
Value |
WHO standard Values |
P-value |
|
Average Drugs per Prescription |
3.6 |
3.6+1.4 |
1.6-1.8 |
<0.001 |
|
Prescriptions with Antibiotics |
560 |
58.3 % |
20.0-26.8 % |
<0.001 |
|
Prescription with Generic |
103 |
10.7 % |
100 % |
<0.001 |
|
Prescription with Injection |
210 |
21.9 % |
13.4-24.1% |
0.123 |
|
Drug from Essential drug list |
586 |
61.04% |
100 % |
<0.001 |
|
Table 3. Prescriptions with omission errors. |
||||
|
Prescription Parameter N=960 |
Number of Prescriptions |
Percentage (%) |
p-value |
|
|
Patient Demographics not mentioned |
Name |
25 |
2.6 |
<0.001 |
|
Age |
572 |
59.9 |
<0.001 |
|
|
Gender |
768 |
80.0 |
<0.001 |
|
|
Weight |
880 |
91.7 |
<0.001 |
|
|
Diagnosis |
460 |
47.9 |
<0.001 |
|
|
Prescriber Details not mentioned |
Prescriber Name |
280 |
29.1 |
<0.001 |
|
Prescriber Qualification |
438 |
45.6 |
<0.001 |
|
|
Address/ Phone number |
461 |
48.0 |
<0.001 |
|
|
Date |
205 |
31.3 |
<0.001 |
|
|
Table 4. Prescriptions with commission errors. |
|||
|
Medication Errors |
No of Prescription |
Percentage (%) |
p-value |
|
Dosage form not Mentioned |
121 |
12.6 |
<0.05 |
|
Dose strength not Mentioned |
245 |
25.5 |
<0.001 |
|
Dose not Mentioned |
163 |
17.0 |
<0.001 |
|
Frequency not Mentioned |
261 |
27.2 |
<0.001 |
|
Duration of therapy not Mentioned |
608 |
63.4 |
<0.001 |
|
Table 5. Prescription errors related to drug-drug interactions. |
||
|
Types of DD interactions |
No of Prescription |
Percentage (%) |
|
Serious |
160 |
16.7 |
|
Moderate |
408 |
42.5 |
|
Minor |
303 |
31.6 |
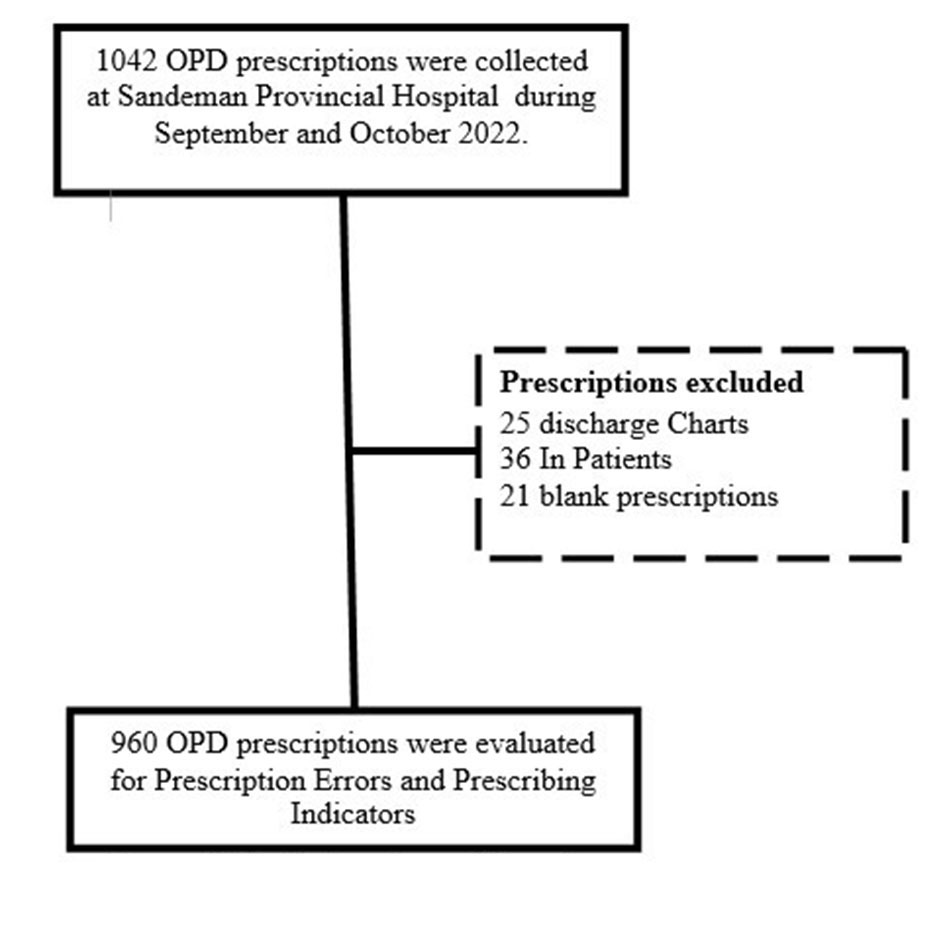 Figure 1. Study duration and flow chart.
Figure 1. Study duration and flow chart.
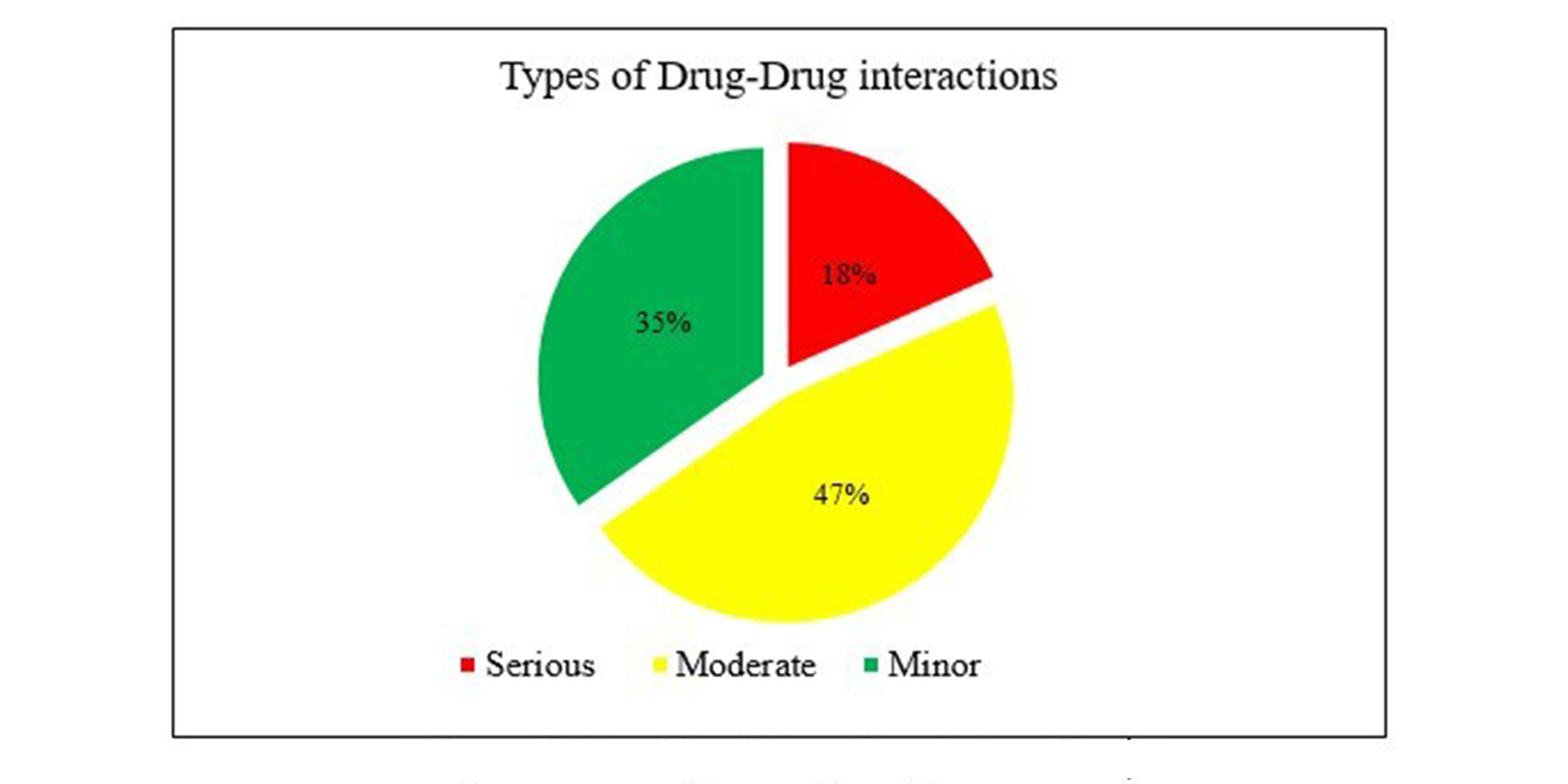 Figure 2. Severity of Drug-Drug interactions.
Figure 2. Severity of Drug-Drug interactions.
The current study found that mean of 3.6 drugs were advised per prescription exceeding the acceptable range (1.6-1.8) drugs per prescription. However lower values were observed in a study conducted in Malawi (1.8) [10] and Zimbabwe (1.3) [11]. On the other hand, studies conducted in India and Nigeria reported (5.6) and (5.2) respectively [12, 13]. Several factors can lead to an increased number of drugs in a prescription. These may include inexperienced physicians, absence of evidence-based practices, incentives for prescribers, insufficient ongoing medical education, and a scarcity of suitable medications. Polypharmacy can negatively impact treatment outcomes as it increases the likelihood of non-compliance and adverse events. Additionally, unnecessary medications can have detrimental effects on healthcare budgets.
The current study found that only 10.7% of prescriptions were written using generic names, far below the optimal value of 100% by WHO. Alarmingly low rates of generic prescribing have also been reported in other countries such as Andorra (6%) [14] and Lebanon (2.9%) [15]. On the other hand, some countries have achieved near-optimal levels of generic prescribing, with rates as high as 92% in Timor-Leste [16] and 98.7% in Ethiopia [12].
Our findings indicate that 58.3% of prescriptions included antibiotics, falling outside the optimal range of 20.0-26.8%. This percentage was comparatively lower in many developing countries, such as Bangladesh (25%) [17] and Brazil (28.8%) [18]. on the other hand, some countries such as Kenya, Timor-Leste and Sudan have higher rates 73.4%, 70%, 70.4% of antibiotic prescribing respectively [17, 18]. Unnecessary antibiotic prescriptions can exacerbate antibiotic resistance, trigger adverse drug reactions (ADRs), and lead to frequent hospitalizations. In our study, 21.9% of prescriptions contained injections, falling within the optimal range of 13.4-24.1%. While this is encouraging, research conducted in Nepal (5.2%) [19] and Angola (4.6%) [18] reported even lower percentages. It's crucial to restrict the use of injections to emergency scenarios, given their higher cost compared to oral medications. Excessive use of injections can also elevate the risk of blood-borne diseases [2].
In our study rate of prescribing drugs from the Essential Drugs List (EDL), at 61.04%, falls below that reported in the Lao People's Democratic Republic and Bangladesh 86.2% and 85% respectively [17, 18]. Rational prescribing requires choosing medications from the EDL, as these drugs are proven, reliable, and frequently more economical than branded options [9]. A prescription mirrors the prescriber's treatment approach and the healthcare system's dynamics within the community [5].
None of the 960 prescriptions analyzed in our study met all the standard prescription criteria. It is crucial to include comprehensive patient information on prescriptions to facilitate accurate dispensing by pharmacists. Patient name is a key identifier on a prescription, while the patient's weight and age are vital for calculating precise doses. Omitting age and weight can hinder pharmacists from reviewing and adjusting treatment regimens. Additionally, specifying gender is essential as certain medications may be effective for one gender but contraindicated for the other. Including the diagnosis in prescriptions, as recommended by WHO, aids pharmacists in interpreting illegible handwriting and ensuring accurate drug dispensing [5]. Remarkably, our study revealed that approximately 91.7% of prescriptions did not include the patient's weight information. Similarly, over 50% and 80% of prescriptions lacked the patient's age and gender, respectively. A study conducted in Saudi Arabia discovered that patients' names, age, gender, and diagnosis were absent in 14.5%, 10%, 4.1%, and 6.8% of prescriptions, respectively. Another study from India indicated that patient age was missing in 11% of prescriptions, gender in 10%, and weight in 100% [20].
Providing comprehensive information about the prescriber is essential in a prescription, as it allows pharmacists and other healthcare professionals to contact the prescriber for clarification or discussion regarding the prescribed medications. The World Health Organization (WHO) advises that each prescription should include thorough details about the prescribers, including their names, addresses, telephone numbers, qualifications, and registration numbers [5].
Ensuring comprehensive information regarding prescribed medications is vital for promoting the rational use of medicines and minimizing prescription errors. Insufficient details about prescribed medicines can lead to under- or over-dosing. Additionally, incomplete treatment regimens may worsen morbidity, while unnecessarily prolonged treatment courses can result in adverse effects, potentially leading to catastrophic outcomes for patients and their families.
The results of this study underscore commission errors present in nearly all prescriptions, with a significant concern being the absence of the duration of therapy in almost 64% of the prescriptions. A study conducted in Bahrain revealed that the duration of treatment was missing in 18.5% of all prescriptions, and frequency information was absent in 3.7% [21]. Similarly, a study from Saudi Arabia indicated that the frequency and number of doses were omitted in 6.9% and 7.6% of total prescriptions, respectively. In an Indian study, it was found that the strength of prescribed medications was not specified in 26.8% of total prescriptions, the number of doses in 35.1%, and the duration of treatment in 26.2% [2].
While medicines play a vital role in healthcare delivery, they also carry inherent risks to patients, including preventable medication errors and unavoidable adverse drug effects (ADEs). Numerous studies have emphasized the impact of ADEs on patient hospitalizations [22, 23]. The risk of ADRs, such as interactions, is often linked to polypharmacy, defined as the simultaneous use of five or more drugs [24]. In this study, the average number of drugs per patient encounter was nearly 4, heightening the likelihood of potential drug interactions (DIs) and ADEs. Approximately 16% of the analyzed prescriptions included major potential drug-drug interactions. Preventing medication errors related to DIs is crucial to mitigate ADEs, as these errors contribute significantly to hospital admissions (3-23%), resulting in increased morbidity and mortality, imposing a considerable financial burden, and presenting a significant public health challenge [25, 26].
This study has some limitations. Firstly, it did not encompass prescriptions originating from private sector hospitals. The Private sector hospitals typically more information to promote the hospital and doctors to have large number of patients. Another constraint of this study pertains to it’s relatively to single hospital attributed to challenges in obtaining consent for data collection from pharmacy managers/owners or patients who were reluctant to share their prescriptions for various reasons.
We thank the Medical Superintendent SPH for allowing to conduct the study, and we are thankful to all the patients who cooperated and provided their prescriptions to be evaluated.
Ethics approval
The ethical committee of Faculty of Pharmacy and Health Sciences University of Balochistan ethically approved the study.
Data availability
The data will be available upon request.
Funding
The authors did not receive any funding or support to report.
Authors’ contribution
Abdul Wahid conceptualized and supervised the study, while Shahbaz Babul, Ghulam Dastagir, M Pervaiz, Shoaib Ahmed collected Munir Ahmed, Shazia Bano, Mahtab Imam entered the data. Abdul Ghafar analyzed the data, and critically reviewed it.
Competing interests
The authors have diligently stated that they have no conflicts of interest to report.
- World Health Organization: How to investigate drug use in health facilities: selected drug use indicators. World Health Organization; 1993 Available from: http://apps.who.int/medicinedocs/en/d/Js2289e/.
- World Health Organization: Promoting rational use of medicines: core components WHO policy perspectives on medicines. World Health Organization; 2002 [cited 2017 July 13]. Available from: http://apps.who. Int/medicinedocs/en/d/Jh3011e/.
- Dean B, Schachter M, Vincent C, Barber N: Prescribing errors in hospital inpatients: their incidence and clinical significance. Qual Safe Health Care 2002, 11(4): 340-344.
- Kopec D, Kabir MH, Reinharth D, Rothschild O, Castiglione JA: Human errors in medical practice: systematic classification and reduction with automated information systems. J Med Syst 2003, 27(4): 297-313.
- De Vries TPGM, Henning R, Hogerzeil HV, Fresle DA: Guide to good prescribing a practical manual. World Health Organization; 1994 Available from: http://apps.who.int/iris/bitstream/10665/ 59001/1/WHO_DAP_94.11.pdf
- Rizwana N, Asif C, Ebrahim ZT: Poaching the (mal) practitioners: DAWN. 2015 Available from: http://www.dawn. Com/news/1203147.
- Punjab Healthcare Commission: PHC Anti quackery strategy. 2013 Available from: https://view.officeapps.live.com/op/view.
- Atif M, Azeem M, Rehan Sarwar M, Malik I, Ahmad W, Hassan F, Rehman A, & Rana M: Evaluation of prescription errors and prescribing indicators in the private practices in Bahawalpur, Pakistan. Journal of the Chinese Medical Association: JCMA 2018, 81(5): 444-449.
- Noman: Aqil 2016 Prescription Pattern of Outpatient Department of a tertiary care Teaching Hospital Quetta, Pakistan.
- Gelders S: Malawi essential drugs program, drug use indicator Survey- 1991. World Health Organization; 1992 [cited 2016 April 27]. Available from: http://apps.who.int/medicinedocs/en/d/Js21679en/.
- Hogerzeil HV, Bimo, Ross-Degnan D, Laing RO, Ofori-Adjei D, Santoso B, Azad Chowdhury AK, Das AM, Kafle KK, Mabadeje AF, et al: Field tests for rational drug use in twelve developing countries. Lancet 1993, 342(8884): 1408-1410.
- Akhtar MS, Vohora D, Pillai KK, Dubey K, Roy MS, Najmi AK, Khanam Razia: Drug prescribing practices in pediatric department of a north Indian university teaching hospital. Asian J Pharm Clin Res 2012, 5(Suppl 1): 146-149.
- Uzoma SON, Lungu A, Ombaka E: Drug use studies in church facilities in Africa. INRUD News 1995, 5: 20.
- Vallano A, Montané E, Arnau JM, Vidal X, Pallarés C, Coll M, Laporte JR: Medical specialty and pattern of medicines prescription. Eur J Clin Pharmacol 2004, 60(10): 725-730.
- Hamadeh GN, Dickerson LM, Saab BR, Major SC: Common prescriptions in ambulatory care in Lebanon. Ann Pharmacother 2001, 35(5): 636-640.
- Chindove S, Ximenes A, Martins N: Medicines prescribing patterns for the treatment of common diseases at community health centers in 3 districts of Timor-Leste. Int J Pharm 2012, 2(3): 439-444.
- Guyon AB, Barman A, Ahmed JU, Ahmed AU, Alam MS: A baseline survey on use of drugs at the primary health care level in Bangladesh. Bull WHO 1994, 72(2): 265-271.
- Holloway KA, Henry D: WHO essential medicines policies and use in developing and transitional countries: an analysis of reported policy implementation and medicines use surveys. PLoS Med 2014, 11(9): e1001724.
- Shankar RP, Pranab KS, Upadhyay DK, Dubey AK, Subish P: Drug utilization among surgical outpatients. TMJ 2006, 56: 230-234.
- Vaishali DP, Deepak BP, Syed Aarif MM, Anjeney M, Saudamini S, Piyush K: Prescription writing practices in a rural tertiary care hospital in Western Maharashtra, India. Australas Med J 2011, 4(1): 4-8.
- Irshaid YM, Al Homrany M, Hamdi AA, Adjepon Yamoah KK, Mahfouz AA: Compliance with good practice in prescription writing at outpatient clinics in Saudi Arabia. East Mediterr Health J 2005, 11(5-6): 922-928.
- Al Khaja KA, Sequeira RP, Al-Ansari TM, Damanhori AH: Prescription writing skills of residents in a family practice residency programme in Bahrain. Postgrad Med J 2008, 84(990): 198-204.
- Beijer HJ, De Blaey CJ: Hospitalisations caused by adverse drug reactions (ADR): a meta-analysis of observational studies. Pharm World Sci 2002, 24(2): 46-54.
- Lazarou J, Pomeranz BH, Corey PN: Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 1998, 279(15): 1200-1205.
- Carbonin P, Pahor M, Bernabei R, Sgadari A: Is age an independent risk factor of adverse drug reactions in hospitalized medical patients? J Am Geriatr Soc 1991, 39(11): 1093-1099.
- Hohl CM, Dankoff J, Colacone A, Afilalo M: Polypharmacy, adverse drug related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Ann Emerg Med 2001, 38(6): 666-671.
Asia-Pacific Journal of Pharmacotherapy & Toxicology
p-ISSN: 2788-6840
e-ISSN: 2788-6859
 Copyright © Asia Pac J Pharmacother Toxicol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Asia Pac J Pharmacother Toxicol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript