Research Article | Open Access
Exploring pharmacist role in dispelling myths regarding covid-19 vaccination
Ayesha Raza Butt1, Hafiz Ur Rehman2, Musa Bin Bashir3, Sandal Khan4
1Department of Pharmacy, Quaid-i-Azam University, Islamabad, Pakistan.
2Trauma Center, Sandeman Provincial Hospital, Quetta, Pakistan.
3 Department Of Cardiology, Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, China.
4Department of Pharmacy, University of Balochistan, Quetta, Pakistan.
Correspondence: Ayesha Raza Butt (Department of Pharmacy, Quaid-i-Azam University, Islamabad, Pakistan; E-mail: royalbolan@gmail.com).
Asia-Pacific Journal of Pharmacotherapy & Toxicology 2024, 4: 1-8. https://doi.org/10.32948/ajpt.2024.02.27
Received: 23 Feb 2024 | Accepted: 02 Mar 2024 | Published online: 02 Mar 2024
Methods A prospective observational study was conducted in two phases at Quaid-i-Azam University (QAU), Islamabad and its peripheral rural area. 200 non-vaccinated individuals were recruited in the pre-intervention phase and 50 in the post-intervention phase. Interview based questionnaire filling was done in both the phases for highlighting the myths causing COVID-19 vaccine hesitancy, and major sources of spreading misinformation. Individuals were guided and counseled regarding misinformation about vaccination.
Results In our study most of the respondents were females (70%). In current study, we counseled 50 participants from pre-intervention phase and significant difference has been seen in percentages. As in the pre-intervention phase, 77% individuals believed the myth that COVID-19 vaccine was developed too fast, and in the post-intervention phase it was reduced to 12% via counseling. Similarly 50% participants believed that vaccine is associated with COVID-19 illness that was decreased to 20%. Highly prevailed myths included too fast development of COVID vaccine (77%), its association with COVID-19 illness (72%), and doubt regarding its efficacy (53%). Chi square analysis found significant association between highly prevailed myths and education level. Study participants with higher education level were more reluctant as they were relying more on the misconceptions regarding COVID-19 vaccine (p-value > 0.05).
Conclusion Awareness regarding misconception and myths via proper counseling played important role in eradicating vaccine hesitancy and optimizing its acceptance. Longer follow up studies on large sample size are required for convincing results.
Key words extra pulmonary TB, TB-high burden country, risk factors, Pakistan
To combat the COVID-19 pandemic, a shielding vaccination is needed to accomplish adequate adaptive immunity against the infection. The significant measure of evolving vaccine is to warrant its safety, because SARS-CoV-2 infection could be boosted by a vaccination if potential risks have been addressed: when infection happens after vaccination is one of the possible risks mentioned in the context of COVID-19 vaccine research [5]. In this COVID-19 pandemic, safe and effective vaccine strategies are of great significance, because vaccine ensures protection due to its capability of triggering a substantial, long-lasting immune response that includes both the neutralizing antibodies and T cells [6].
People’s refusal to receive nonviolent and suggested vaccines is called “vaccine hesitancy”. To increase the vaccine uptake, foremost step is to determine the reason behind the hesitation of people towards vaccination [7]. According to the studies conducted worldwide, people are vaccine hesitant because of their concern related to the side effects, and doubts regarding the safety and efficacy of vaccines. Extensive availability of smartphones have made easy access to the internet; and social media has pros and cons. In vaccine decision-making process, it might be valuable tool for self-education but significant disadvantages such as misinformation and myth about COVID-19 vaccine are not comprehensible [7].
People who doubt the safety of COVID-19 vaccine are not willing to receive it; lack of the information regarding virus is the prime reason behind accepting the vaccine related myths [8]. To eradicate COVID-19, it is important that maximum number of people get vaccinated, but the fast spread of misinformation and myths regarding Corona vaccination are massive hurdles in the immunization process. Aim of this study is to dispel the misinformation and to optimize the vaccine acceptance by highlighting the myths that contribute to increase reluctance to the COVID-19 vaccination, and to educate and counsel the individuals breaking the shackles of misinformation.
A prospective observational study was conducted to observe the misinformation causing COVID-19 vaccine hesitancy and to optimize the vaccine acceptance through counseling and educating individuals. The targeted study population included people who were non-vaccinated against COVID-19. The data was collected from the students of Quaid-i-Azam University, Islamabad, Pakistan and from the peripheral rural areas of University. The study duration was three months from Jun-Aug 2021.
Inclusion & exclusion criteria
The non-vaccinated individuals in the rural areas and university premises were included in the study, while all the people already vaccinated against COVID-19 were excluded.
Sample size
Non-probability convenience sampling technique was used for enrolment of the study population. All individuals meeting inclusion/exclusion criteria during study duration in pre intervention were 200 and in post-intervention were 50.
Study tool
The questionnaire was self-designed and pre-validated by the 3 experts of relevant field before the start of original research. The questionnaire comprised of 2 parts, first part included demographics details (i.e., gender, employment status, education, family income and residence) and disease history. The second part of questionnaire included of two sections; one about the perception of people towards myth regarding COVID-19 vaccine i.e. refusal, development, safety, fear, death, immunity, protection, illness, efficacy, symptoms, wait, data, weapon, area, registration, infertility, brand, nano-chip and population control, and other section was to observe major sources of spreading myths i.e. social media, television, family/friends, never heard before, other and all. Interview based questionnaire filling has been done in both pre and post intervention phases and individuals were guided and counselled.
Data collection
One-to-one interview was conducted with non-vaccinated participants in pre-intervention phase and the response was noted on the questionnaire. Immediately after getting responses, individuals were counselled and guided regarding their queries and misconceptions while explicating their feedbacks. Later in couple of weeks, few of those individuals were indulged in post intervention phase to get reciprocated responses. However, sample size was finite due to limited time span of survey. Figure 1 shows the study flowchart.
Statistical analysis
Statistical software package for social sciences (IBM SPSS Statistical version 20) has been used to analyze data. Percentages and frequencies were used for depicting categorical variables using simple descriptive statistics. Chi Square Independent test was used to analyze significant association between highly prevailed myths in study population and education level. P-value less than 0.05 was considered as statistically significant.
After the inclusion of eligible respondents, we used the following workflow diagram during data collection is shown in Figure 2.
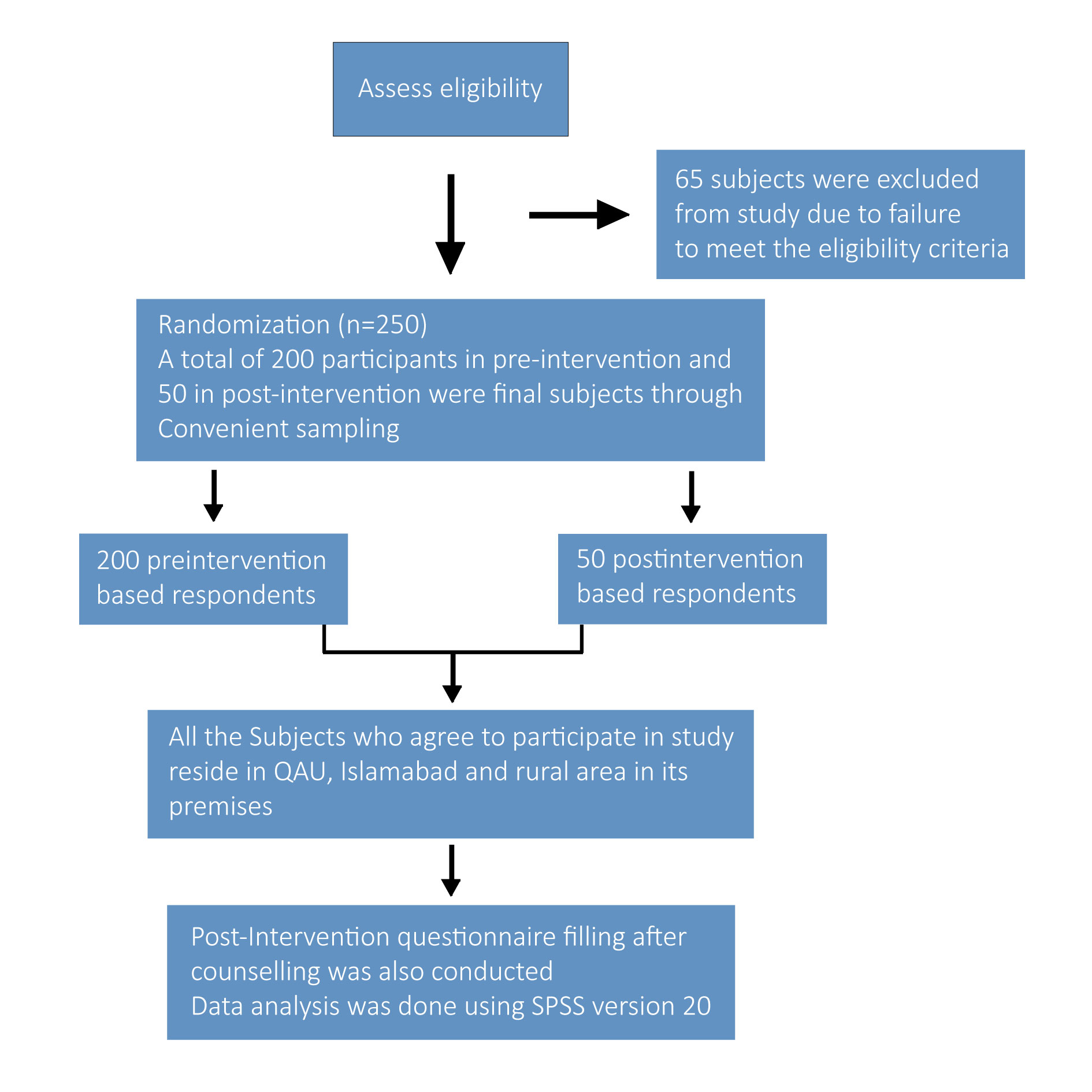 Figure 1. Study flow chart.
Figure 1. Study flow chart.
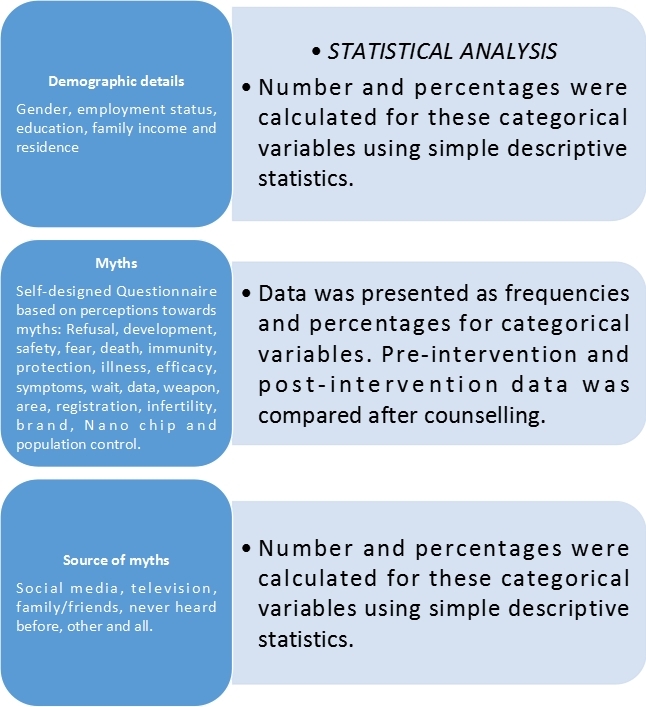 Figure 2. Study work flow.
Figure 2. Study work flow.
Demographics of study population included gender, age, occupation, education, family income and residence status is presented in Table 1.
Myths contributing to COVID-19 vaccine hesitancy
Perception of study population toward the myths regarding COVID-19 vaccine were related to its safety, efficacy, post-vaccination complications, death, political conspiracy, infertility, insufficient information about vaccination center and lack of knowledge associated with its registration. Table 2 highlights the myths with frequency and percentage of the pre and post-intervention phase.
Association between highly prevailed myths and education level
Chi-Square analysis was performed to find association of highly prevailed myths in study population with their education level. Study participants with higher education level was found abundant in number who were more hesitant to vaccine because of their strong believe on misinformation and myths related to COVID-19 vaccine. Variables having p-value less than 0.05 were assessed as shown in Table 3.
Major source of spreading misinformation
Summary statistics of major source of spreading misinformation. In study group was social media (46%), television (8%), family/friends (12%), all three (31%), other (2%) and never heard before (1%).
|
Table 1. Demographics of non-vaccinated study participants (n=200). |
|||
|
Sr. No. |
Demographic Variables |
Categories |
Number (percentage)
|
|
1 |
Gender |
Male |
60 (30) |
|
Female |
140 (70) |
||
|
2 |
Age |
15-26 |
112 (56) |
|
27-38 |
45 (22.5) |
||
|
39-50 |
28 (14) |
||
|
51-62 |
12 (6) |
||
|
63-74 |
3 (1.5%) |
||
|
3 |
Employment Status |
Govt. Employed |
54 (24) |
|
Private Employed |
24 (12) |
||
|
Unemployed |
122 (51) |
||
|
4 |
Education |
Primary |
18 (9) |
|
Secondary |
57 (28.5) |
||
|
Intermediate |
26 (13) |
||
|
Above |
99 (49) |
||
|
5 |
Family Income |
Low |
21 (10.5) |
|
Moderate |
146 (73) |
||
|
High |
33 (16.5) |
||
|
|
Residence |
Rural |
57 (28.5) |
|
Urban |
143 (71.5) |
||
|
Table 2. Myths regarding COVID-19 vaccine (pre-intervention phase and post-intervention). |
||||||
|
Sr. No. |
Myths about COVID-19 Vaccine |
Categories |
Frequencies(Pre-Intervention Phase (n=200)/Post-Intervention Phase (n=50) |
Percentage(Pre-Intervention Phase/Post-Intervention Phase |
||
|
1. |
Do you think COVID-19 Vaccine was developed too fast? |
Yes |
154 |
6 |
77% |
12% |
|
No |
46 |
44 |
23% |
88% |
||
|
2. |
Do you think it is not safe for your health? |
Yes |
92 |
12 |
46% |
24% |
|
No |
108 |
38 |
54% |
76% |
||
|
3. |
Are you scared of post vaccination complications? |
Yes |
80 |
12 |
40% |
40% |
|
No |
120 |
38 |
60% |
60% |
||
|
4. |
Do you think you would die after being vaccinated? |
Yes |
34 |
8 |
17% |
16% |
|
No |
166 |
42 |
83% |
84% |
||
|
5. |
Do you think your physiological immunity is better? |
Yes |
151 |
16 |
75.5% |
32% |
|
No |
49 |
34 |
24.5% |
68% |
||
|
6. |
Do you think it will not provide long-term protection? |
Yes |
100 |
9 |
50% |
18% |
|
No |
100 |
41 |
50% |
82% |
||
|
7. |
Do you think it is associated with COVID-19 illness? |
Yes |
144 |
10 |
72% |
20% |
|
No |
56 |
40 |
28% |
80% |
||
|
8. |
Do you Doubt regarding vaccine efficacy? |
Yes |
106 |
10 |
53% |
20% |
|
No |
94 |
40 |
47% |
80% |
||
|
9. |
Do you think COVID-19 symptoms are mostly mild? |
Yes |
54 |
12 |
27% |
24% |
|
No |
146 |
38 |
73% |
76% |
||
|
10. |
Are you waiting for others to vaccinate first? |
Yes |
77 |
4 |
38.5% |
8% |
|
No |
123 |
46 |
61.5% |
92% |
||
|
11. |
Do you think it is not safe until we get more long-term data? |
Yes |
145 |
7 |
72.5% |
14% |
|
No |
55 |
43 |
27.5% |
86% |
||
|
12. |
Do you think it is a political weapon to harm Muslim Nation? |
Yes |
55 |
5 |
27.5% |
10% |
|
No |
145 |
45 |
72.5% |
90% |
||
|
13. |
You did not know where to be vaccinated? |
Yes |
93 |
9 |
46.5% |
18% |
|
No |
107 |
41 |
53.5% |
82% |
||
|
14. |
You did not know the procedure of being registered? |
Yes |
90 |
10 |
45% |
20% |
|
No |
110 |
40 |
53.5% |
80% |
||
|
15. |
Do you consider it unnecessary to fight against COVID-19? |
Yes |
59 |
11 |
29.5% |
22% |
|
No |
140 |
39 |
70% |
78% |
||
|
16. |
Do you think vaccine could lead to infertility? |
Yes |
39 |
4 |
19.5% |
8% |
|
No |
161 |
46 |
80.5% |
92% |
||
|
17. |
Are you perplexing about different vaccine brands? |
Yes |
145 |
9 |
72.5% |
18% |
|
No |
55 |
41 |
27.5% |
82% |
||
|
18. |
Do you think its installation of 5G Nano-Chips in human to control them? |
Yes |
35 |
3 |
17.5% |
6% |
|
No |
165 |
47 |
82.5% |
94% |
||
|
19. |
Do you think it is created to control world population? |
Yes |
69 |
8 |
34.5% |
16% |
|
No |
131 |
42 |
65.5% |
86% |
||
|
Table 3. Association between myths and education level. |
||||||
|
Myths about COVID-19 Vaccine |
Categories |
Primary Education level (n=18) |
Secondary Education level (n=57) |
Inter-mediate Education level (n=26) |
Above (n=99) |
P-value (p<0.05) |
|
Do you think COVID-19 Vaccine was developed too fast? |
Yes |
9 |
44 |
21 |
80 |
0.038 |
|
No |
9 |
13 |
5 |
19 |
||
|
Do you think it is associated with COVID-19 illness? |
Yes |
9 |
49 |
23 |
63 |
0.001 |
|
No |
9 |
8 |
3 |
36 |
||
|
Do you Doubt regarding vaccine efficacy? |
Yes |
8 |
27 |
9 |
62 |
0.037 |
|
No |
10 |
30 |
17 |
37 |
||
|
You did not know the procedure of being registered? |
Yes |
8 |
38 |
11 |
33 |
0.001 |
|
No |
10 |
19 |
15 |
66 |
||
In 2021, national survey was conducted in USA regarding COVID-19 vaccine acceptance which concluded that doubts related to safety and lack of knowledge about virus are the main reasons of vaccine hesitancy and trusting myths. People more hesitant to vaccine were those having less education and lower income and those belonging to rural areas; and study found that better communication with them can eradicate the knowledge gap in different socioeconomic and educational background[13, 14]. Our study highlighted the myths among students of QAU and in its rural premises (n=200). Highly prevailed myths included; too fast development of COVID vaccine (77%), its association with COVID-19 illness (72%), and doubt regarding its efficacy (53%). Significant association was found between these myths and education level, as study participants with higher education level were more reluctant to vaccine due to trusting myths (p<0.05).
According to the other studies conducted worldwide, people are vaccine hesitant because of their concerns related to side effects, and doubts regarding safety and efficacy of vaccines. Extensive availability of smartphones have made easy access to the internet and social media have pros and cons. In vaccine decision-making process it might be a valuable tool for self-education, but significant disadvantage; such as, misinformation and myths about COVID-19 vaccine are not comprehensible [15-17]. Our results concluded that social media (46%) is the major source of spreading misinformation.
A study related to COVID vaccine hesitancy showed that the novelty of vaccine (82%) and fear of side effects (80%) are the main reasons of declining rate of COVID-19 vaccination. Not only the effective vaccine is required but also the effective strategies for implementation; and policymakers may reduce vaccine hesitancy through campaigns to increase the public awareness and to raise confidence in the safety and efficacy of vaccine [18, 19]. In current study, we counseled 50 participants from pre-intervention phase and significant difference has been seen in percentages. As in the pre-intervention phase, 77% individuals believed the myth that COVID-19 vaccine was developed too fast, and in the post-intervention phase it was reduced to 12% via counseling. Similarly 50% participants believed that vaccine is associated with COVID-19 illness that was decreased to 20%. Frequent decline has been seen in believing myths in the post-intervention phase. Hence, education and guidance plays a vital role in eradicating hurdles regarding vaccine acceptance and increases NO. of vaccinated people which indirectly is a useful tool to combat COVID-19 pandemic.
Study Limitations: In limited period, no long-term follow up study has been managed. Hence, longitudinal method to evaluate changed perceptions related to time and different analysis methods to find association with misinformation is needed as convincing evidence.
We are grateful to the Department of Pharmacy, Quaid-i-Azam University for the support rendered to ensure the success of this study.
Ethics approval
The ethical approval was obtained from ERB of Department of Pharmacy Quaid I Azam University, Islamabad for being a project of post-graduation. Additionally, informed consent from the respondents was also obtained.
Data availability
All relevant data are within the paper.
Funding
The author(s) received no specific funding for this work.
Authors’ contribution
Ayesha Raza Butt collected the data, conceptualized, supervised the study. Hafeez Ur Rehman analyzed the data and proofread manuscript, Sandal Khan entered data. Musa Bin Bashir wrote the manuscript.
Competing interests
The authors have declared that no competing interest exist.
- Ashok K, Babu M, Satheesh D: Health Management Crisis of COVID-19. Adv Chem Res 2023, Epub ahead of print.: 89-101.
- Vijay R, Perlman S: Middle East respiratory syndrome and severe acute respiratory syndrome. Curr Opin Virol 2016, 16: 70-76.
- Park SE: Epidemiology, virology, and clinical features of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clin Exp Ped 2020, 63(4): 119-124.
- Ciotti M, Ciccozzi M, Terrinoni A, Jiang W-C, Wang C-B, Bernardini S: The COVID-19 pandemic. Crit Rev Clin Lab Sci 2020, 57(6): 365-388.
- Haynes BF, Corey L, Fernandes P, Gilbert PB, Hotez PJ, Rao S, Santos MR, Schuitemaker H, Watson M, Arvin A: Prospects for a safe COVID-19 vaccine. Sci Transl Med 2020, 12(568): eabe0948.
- Jeyanathan M, Afkhami S, Smaill F, Miller MS, Lichty BD, Xing Z: Immunological considerations for COVID-19 vaccine strategies. Nat Rev Immunol 2020, 20(10): 615-632.
- Machingaidze S, Wiysonge CS: Understanding COVID-19 vaccine hesitancy. Nat Med 2021, 27(8): 1338-1339.
- Kricorian K, Civen R, Equils O: COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccin & Immunother 2022, 18(1): 1950504.
- Kaur SP, Gupta V: COVID-19 Vaccine: A comprehensive status report. Virus Res 2020, 288: 198114.
- Sadarangani M, Marchant A, Kollmann TR: Immunological mechanisms of vaccine-induced protection against COVID-19 in humans. Nat Rev Immunol 2021, 21(8): 475-484.
- Sallam M: COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines 2021, 9(2): 160.
- Rutten LJF, Zhu X, Leppin AL, Ridgeway JL, Swift MD, Griffin JM, St Sauver JL, Virk A, Jacobson RM: Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. In: Mayo Clinic Proceedings: 2021: Elsevier; 2021: 699-707.
- Kriss JL, Hung M-C, Srivastav A, Black CL, Lindley MC, Lee JT, Koppaka R, Tsai Y, Lu P-J, Yankey D: COVID-19 vaccination coverage, by race and ethnicity—national immunization survey adult COVID module, United States, December 2020–November 2021. MMWR Morb Mortal Wkly Rep 2022, 71(23): 757-763.
- Miller M, Zhang W, Azrael D: Firearm purchasing during the COVID-19 pandemic: results from the 2021 National Firearms Survey. Ann Inter Med 2022, 175(2): 219-225.
- Cuan-Baltazar JY, Muñoz-Perez MJ, Robledo-Vega C, Pérez-Zepeda MF, Soto-Vega E: Misinformation of COVID-19 on the internet: infodemiology study. JMIR Public Health Surveill 2020, 6(2): e18444.
- Skafle I, Nordahl-Hansen A, Quintana DS, Wynn R, Gabarron E: Misinformation about COVID-19 vaccines on social media: rapid review. J Med Int Res 2022, 24(8): e37367.
- Bin Naeem S, Kamel Boulos MN: COVID-19 misinformation online and health literacy: a brief overview. Int J Environ Res Public Health 2021, 18(15): 8091.
- Luo F, Ghanei Gheshlagh R, Dalvand S, Saedmoucheshi S, Li Q: Systematic review and meta-analysis of fear of COVID-19. Front Psychol 2021, 12: 661078.
- Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM: Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J Anxiety Disord 2020, 74: 102258.
Asia-Pacific Journal of Pharmacotherapy & Toxicology
p-ISSN: 2788-6840
e-ISSN: 2788-6859
 Copyright © Asia Pac J Pharmacother Toxicol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Asia Pac J Pharmacother Toxicol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript